Fairfield alumni in nursing and health professions at the forefront of the fight against covid-19
In this time of isolation, i hope our patients never feel alone with a nurse present. through a simple touch or hold of the hand, i do everything in my power to make sure my patients feel the love they deserve.
— Cara Gibbons ’18, RN
The sound of chimes plays overhead at North Shore University Hospital in Manhasset, New York, as its one-thousandth patient diagnosed with the coronavirus is discharged. It is part of a program, introduced by the hospital, called “Chimes of Hope.”
“This is truly an exciting moment for everyone at the hospital. It signifies how well all of the work and sacrifice are working. It makes the long, tiring shifts meaningful. We will get through this, and it will make us stronger,” said ICU nurse Cara Gibbons ’18, RN. As the coronavirus pandemic first swept across the United States, medical professionals around the nation — including the many thousands of Fairfield alumni who work in nursing and health care — were forced to adapt to a new reality just as quickly and intensely as the virus was spreading. Likening their work to going to war, they faced profound challenges.
“This particular patient population we are working with requires especially diligent monitoring,” noted Gibbons. “Even the most experienced health care professionals remain uncertain of the proper prognosis and treatment plans. However, we are all determined to find the answer.”
When she arrives for her night shift, Gibbons immediately picks up a pair of hospital-issued scrubs and a paper bag that contains her N95 mask, goggles, and a face shield she will wear for the next 12 hours. Feeling nervous, but honored to be serving others during this pandemic, she looks at the ICU assignment sheet for her shift.

Alexandra Antonacci ’15, RN and coworkers came together at New York-Presbyterian Hospital/Weill Medical Center.
The care tasks for each Covid-19 patient include providing nourishment, administering medications, turning and repositioning, close monitoring for sedation, ensuring ventilator compliance, drawing blood, and dialysis.
“Our patients are at all different progressions of the virus while we care for them. During each stage of the disease, patients require differing support. We still look at each of our patients as unique individuals who require precise attentiveness to their needs,” said Gibbons.
While undergoing treatment, Covid-19 patients are kept in isolation and family members are unable to visit. To address this challenge, the nurses update family members by phone and also have them fill out questionnaires to learn more about the patients. Knowing personal details, like favorite music or nicknames, allows nurses to connect with patients and takes away some of the loneliness of isolation.

Cara Gibbons ’18, RN (on right) and Veena Cherian, RN are ICU nurses at North Shore University Hospital in Manhasset, N.Y.
“Three of my generous colleagues began offering to visit patients in the hospital, to relay messages from their families,” Gibbons shared. “In this time of isolation, I hope our patients never feel alone with a nurse present. Through a simple touch or hold of the hand, I do everything in my power to make sure my patients feel the love they deserve.”
At New York-Presbyterian Hospital/Weill Cornell Medical Center, each person who enters the facility — doctors, nurses, and walk-ins — receives a facemask to be used for the remainder of the day. Pediatric Intensive Care (PICU) nurse Alexandra Antonacci ’15, RN, regularly stores her mask for reuse.
“If a mask isn’t visibly soiled or stretched to the point that the seal isn’t suitable anymore, I will save it, disinfect it, and reuse it in the future.”
When the pandemic hit New York City, Antonacci and her fellow nurses converted their PICU unit into a Medical Intensive Care Unit (MICU), and received adult intensive care training in a matter of days.
“All of our PICU nurses floated around our hospital, to various adult ICUs, to train. We knew we were ICU nurses and could do this, but were unsure of what taking care of an adult meant,” said Antonacci.
Her PICU was transformed into a 23-bed intensive care unit, with three of the beds designated for neonatal intensive care. Patients were set up in negative pressure rooms, to keep the virus contained, while the nurses were kept in a positive pressure room. When the unit was converted, windows were installed to allow the nurses to sit in the rooms with their patients.
“As pediatric ICU nurses, we are used to sitting in our patient’s room and not really having to think about how often we are coming in contact with our patients, because until now, they were never a real threat to us,” she said.
Her shift begins at 7:30 a.m. After a quick huddle with the charge nurse to go over the schedule and any changes for the day, she goes to her assigned room where she gets a report from the night nurse. Because every patient is Covid-positive, the rest of the day is spent leaving and re-entering the room as few times as possible.
“This goes on for about 12 hours of our day, with limited bathroom breaks and water breaks. Gowning to go into the room takes a decent amount of time, and in order to be safe, it’s important to be meticulous about taking off your personal protective equipment so that the virus does not spread or contaminate anything, before exiting the room.”

Antonacci and her unit employ a variety of treatment options for their patients. She explained, “Whenever a new medication, or trial, or anything comes out that we think can help our patients beat this disease — we try it. Right now there are a lot of unknowns, but we are keeping up with the research and not afraid to try things we’ve never done before.”
At the end of her 12-hour shift, she cleans her masks and goggles with designated wipes, and washes her hands one last time. She places her mask in the same paper bag she started her day with and returns it to her locker. She says goodbye to her co-workers, whom she will see again the next morning, in what she describes as their “new normal.”
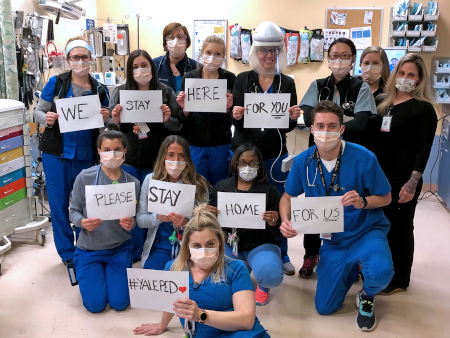
For Nicholas Mudry ’17, RN, a pediatric emergency room nurse at Yale-New Haven Hospital who is also currently pursuing a doctor of nursing practice–family nurse practitioner degree (DNP-FNP) at Fairfield, it is the uncertainty that is the biggest challenge.
“It is a nerve-wracking time to be working in a hospital. There is a lot of uncertainty, and protocols are constantly changing as new information is being discovered about the coronavirus,” he said. “What I have found to be the biggest worry for most nurses is not necessarily being exposed to the coronavirus themselves, but bringing it home to their families.”
At Yale-New Haven Hospital, every day is different in the emergency room, depending on a number of variables including a rotating daily assignment (triage nurse, trauma nurse, bedside nurse, etc.) and the volume and acuity of patients.
“There is always a little bit of anxiety going into a shift, as there is a sense of uncertainty about what the day will be like and what kind of patients you will be taking care of,” he said. “There are days where you barely have the time to sit down, as there is constantly something that needs to be done. However, through all of that, I feel a sense of accomplishment — that I did everything I could to provide the best care for my patients.”
At the onset of the pandemic, Yale-New Haven Hospital installed a tent outside the Emergency department for triage, in the hopes of discharging patients without having them enter the hospital and risk exposure to the virus. When assessing patients, they treat anyone with a fever or respiratory symptoms as a possible Covid-19 case.
“I feel like being a nurse on the front line is a mindset. You have to be willing to work hard, adapt, and do what is best for the patient no matter what, while also keeping yourself safe and healthy. We all have a common enemy, and are doing everything we can to overcome it.”
At Bridgeport Hospital, Fairfield DNP candidate Jennifer Dellemonico, RN, CEN, is testing patients through the hospital’s drive-through testing site. The emergency room has had multiple cases of Covid-19 requiring admission to the ICU floor. The drive-through testing allows health care workers to swab patients in their cars and send them home to quarantine until their results come in.
Dellemonico and her colleagues have their temperatures taken at the start of each shift, before putting on their N95 masks and face shields. Though at the time of this writing in late April they are currently seeing fewer patients each day, the acuities are higher and patients are requiring more care.
“We are used to dealing with chaos, but this is unknown territory,” Dellemonico said. “Our day-to-day operations have been completely turned upside down. The thought of running out of PPE is always on our minds, and many ER nurses are being sent to help in the ICUs. Even though this is not our comfort zone — and a huge learning experience — we are here to help and happy to be on the front line helping these patients.”
Guided by the Jesuit emphases on social responsibility, reflection, and lifelong learning, the Marion Peckham Egan School of Nursing and Health Studies develops leaders who demonstrate excellence across environments of care, which is evident in the many alumni currently serving on the front lines of this pandemic.
As our Egan School alumni continue to treat coronavirus patients, they all have one thing in common: despite the sudden onset of this pandemic, they feel prepared to tackle it head-on.
Antonacci explained, “The Egan School has prepared me by teaching me the absolute fundamentals of being a nurse. I don’t think there is anything that can truly prepare you for a pandemic like this, but I became a nurse with the training of the incredible professors at Fairfield University and for that I am beyond grateful. This may be a devastating time for many, but there’s nowhere I would rather be than bedside, helping these very sick patients.”